It’s Time to Heal is a special package about engineering the future of bio and healthcare. See more at: https://a16z.com/time-to-heal/.
2020 was the year virtual care went mainstream. Given this new visibility — and the confluence of strong regulatory, behavioral and technical tailwinds — it is easier and more attractive than ever to stand up a virtual clinic.
But not all virtual care models are created equal, or have equal benefits to patients. Entrepreneurs and operators building this next generation of virtual clinics must ensure that the level of care provided equals — or better yet, exceeds — that of brick-and-mortar counterparts. So how do builders in this space guarantee the highest level of care? I believe that it is by valuing and integrating clinical rigor throughout.
In this piece, I will break down what it means to be clinically rigorous in this virtual care context, how this creates a flywheel that benefits patients and creates the strongest and most durable business models, and lastly, how technology is enabling clinical rigor in ways that are inaccessible to traditional care models.
What is clinical rigor?
The term clinical rigor typically triggers mental images of peer-reviewed journal articles and is often synonymous with methodological rigor and reproducibility for specific clinical interventions. While this version of rigor is a critical piece of a virtual care model, an expanded mental model of clinical rigor is important to drive durable, sustainable impact on the health and well-being of patients.
Clinical rigor can also be thought of as the clinic being rigorous. That is, an end-to-end care model — not just an isolated intervention — that can: (1) reliably deliver high-value care, (2) create a positive patient experience, and (3) continually improve over time. With that lens, clinical rigor goes far beyond the validation of the specific intervention and permeates into the entire care model, from the design of the patient-doctor interaction, to the business model, to the organizational structure of the company. Taken this way, clinical rigor is part of the core ethos and fabric of the company.
Clinical rigor can also be thought of as the *clinic* being *rigorous*.When I am evaluating the clinical rigor of a virtual care model, I ask the following questions:
- Does it apply interventions that are best practice and have been shown to be safe and effective?
- Does it apply a patient-centric lens in the design of the care experience?
- Does it track process and outcome measures while also assessing for unintended consequences?
- Can those process and outcome measures be directly tied to an impact on total cost of care or other economic ROI drivers?
- Does it appropriately match the clinical resource (person delivering the care, site of care, modality of care) with the patient needs?
- Does it facilitate real-time learning, care model refinement, and eventual evidence generation at an individual and population level?
- Does it integrate with other aspects of an individual’s care journey and consider transitions in care where appropriate?
It’s unrealistic to expect that virtual care companies will check every one of these boxes from day one, but having the strategic and product roadmaps of the company aligned to these as true north will pay dividends at each stage of the company’s growth.
Why should virtual care companies care?
It is clear how integrating clinical rigor into a virtual care model will, by definition, drive differentiated clinical outcomes for patients. But perhaps less obvious but equally important, is its role in building transformational, durable businesses in healthcare.
A confluence of tailwinds has accelerated the uptake of virtual care in a way many would not have predicted. Numerous companies are experiencing immense growth by solving access challenges and relieving pent up patient demand. The quickly maturing virtual care tech stack is also enabling this shift. But, just like we are seeing with legacy care models, we anticipate a transition from volume to value in virtual models. Successfully navigating this shift from fee-for-service to value-driven constructs (like pay-for-performance, centers of excellence, bundled payments, and full capitation) will require extensive integration of clinical rigor into all levels of the care and business model.
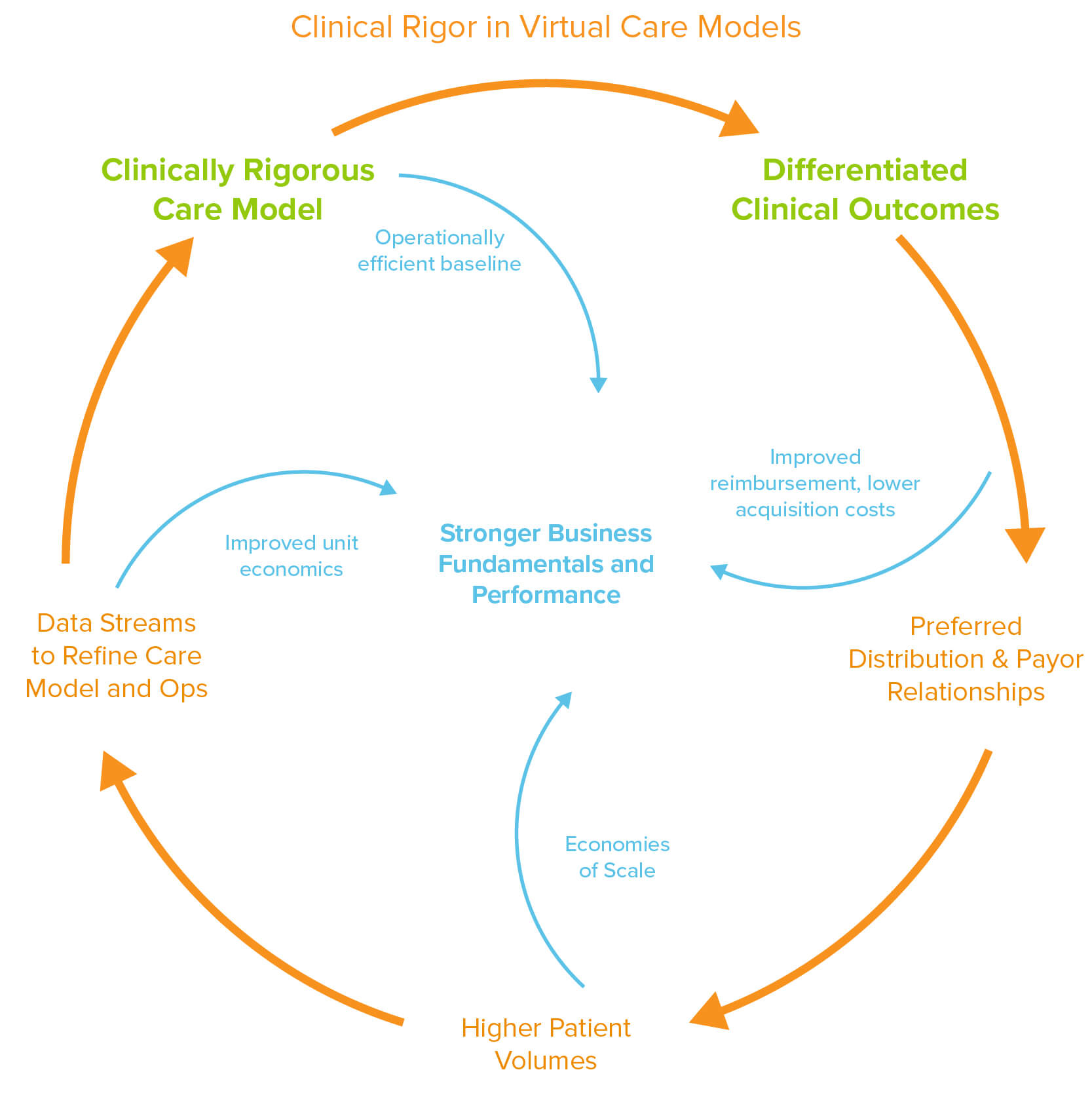
Successfully navigating this shift from fee-for-service to value-driven constructs will require extensive integration of clinical rigor into all levels of the care and business model.I believe that the most impactful models will be those that build on the flywheel of a clinically rigorous model. This flywheel can take a variety of shapes, but in a generalized form can be thought of as:
We are seeing this flywheel start to spin for a number of companies. For example, we have seen a handful of companies parlay differentiated clinical outcomes into preferred (semi-exclusive) provider relationships with payors, leading to simplified patient acquisition channels and higher reimbursement rates. This near-term success can drive long-term impact by activating this feed-forward loop as preferred relationships drive higher patient volumes, which leads to more data to refine the care model both clinically and operationally. A more refined care model then leads to even further differentiated clinical outcomes on top of better operational efficiency and business fundamentals. As competition in virtual care continues to rise, I see this as being a viable path to defensibility long-term.
There are parts of the virtual care ecosystem where clinical rigor is table stakes (e.g. products sold to payors or at-risk groups as carve out offerings). However, the huge recent push towards virtual care has unlocked and accelerated paths to scale in other parts of the virtual care ecosystem which demand less attention to clinical rigor at the outset. While enticing to build aggressively in these areas, this can create a large amount of what I think of as “clinical debt” that will eventually be called in.
We have already seen this start to play out in several areas of the market, with a prime example being remote patient monitoring (RPM). When the novel RPM reimbursement codes were launched in late 2019, there was a flurry of activity as companies sprung up using the new codes as a long awaited business model scaffold for remote care. These companies exhibited a wide range of attention to clinical rigor with some broadly deploying RPM devices without clear ties into a surrounding clinically rigorous model. Over the past several weeks, however, CMS has clarified and tightened the guidelines around the RPM codes. Will less rigorous models be able to meet these new (and future) guideline updates? Time will tell, but by not investing in clinical rigor at the outset, they are now exposed to existential risk. More broadly, this move is a clear signal that CMS (and other payors) will increasingly demand and reward higher-value, more clinically rigorous care models.
How is tech enabling clinical rigor?
One of the most exciting features of virtual care companies is that, in many ways, they are better positioned to deploy clinically rigorous care models than their brick-and-mortar analogs. Here are a few ways that I see tech enabling clinical rigor:
- Gathering clinical and operational metrics: data architectures within virtual care models can enable the passive collection of much more granular clinical and operational data. This can lead to more continuous measurement of clinical processes and outcome measures and can even unlock new methods of clinical assessment. On the operational side, data can be captured from every internal and patient-facing interaction leading to increased visibility into operational efficiency.
- Learning and refining the care model: coupling the granular clinical and operational data feeds can unlock continuous learning through a closed loop between inputs (resources, interventions) and outputs (clinical/cost outcomes). Over time, this can become a path to evidence generation and defining new best practice.
- Scaling the provider: virtual care stacks are inherently more modular and amenable to augmentation/automation which can enable providers to more efficiently care for a patient population while also potentially reducing burden. This coupled with a closed loop learning model can drive more precise matching between patient needs and the right care modality (type of provider, “site” of care, delivery method, care intervention, etc).
- Improving integration with other aspects of care: lower friction-flows of patient data and communication between care team members both internally and externally can enable more holistic patient care, better care collaboration/coordination, dynamic care supervision across care teams, and more seamless consultations/referrals.
- Patient experience design: no longer is it science fiction to imagine a world where the patient care experience is more reminiscent of our favorite consumer apps than going to the DMV. The impact of this can extend beyond patient satisfaction scores to more meaningful engagement and adherence over time.
With the various technical, regulatory, and behavioral tailwinds aligning behind virtual care, I couldn’t be more excited about the opportunity to launch and scale clinically rigorous virtual care models. I see a unique window to not only drive significant patient impact, but also build a new generation of transformative healthcare companies. It’s time to build in virtual care.