Half-Priced Healthcare That’s Twice as Good
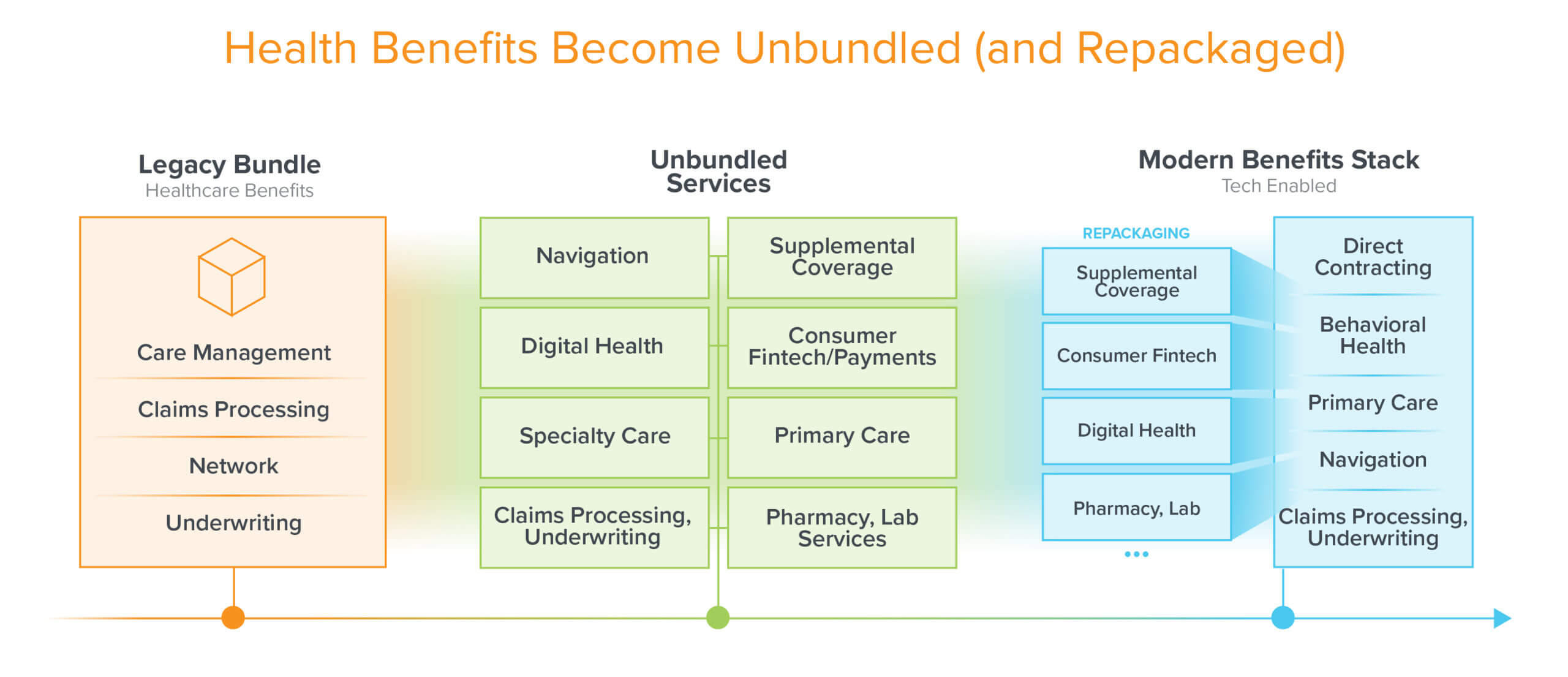
Health insurance is undergoing a rapid cycle of unbundling and repackaging. Vertically-integrated “payviders” (groups that both pay for services, like an insurer would, and administer those services, like a provider would) are emerging as a new standard, and provider networks are being recontoured as virtual-first care models take root. The monolithic products of legacy insurance companies and third-party administrators (TPAs) are quickly being replaced with efficient, tech-enabled upstarts that perform high-resolution underwriting and automated claims processing, real-time payments and modular network management, and multi-channel member engagement. This is all in response to the untenable healthcare cost trends we’ve experienced over the last decade, during which family insurance premiums rose more than 54%, and deductibles more than 160%.
We’ve written before about the critical importance of primary care in value-based payments models, given its ability to intervene early at lower cost, and mitigate downstream spikes in high-acuity clinical events and spend. Because of this central role, virtual-first primary care is becoming a core, integrated pillar of modern insurance products – 89% of employer health benefits plans included coverage for low-acuity telehealth in 2020, up from only 27% just 5 years ago. The competition in this category is also growing rapidly, driving the bar ever higher for what defines truly advanced primary care.
To that end, we believe virtual-first primary care needs to incorporate the following capabilities to be able to compete in this fast evolving marketplace:
- Embedded navigation services to quarterback all parts of the healthcare journey
- Tight integration with IRL services, whether on-site or home-based
- Integrated virtual-first behavioral health, pharmacy, and lab services
- An operationalized specialty care network (not just a static list of specialists with phone numbers!), curated based on performance, and with direct contracts and tightly enforced service level agreements
- A tech stack that treats the care team, the patient, AND referral partners as primary users
Top-performing primary care groups need these cutting-edge capabilities to manage costs, bear risk in value-based payment schemes, and ultimately deliver accountable, cost-effective care – in other words, “half-priced healthcare that’s twice as good, clinically and emotionally” which is the goal and founding principle of Firefly Health.
Firefly Health was founded by advanced primary care expert Dr. Andy Ellner and digital health innovation leader Dr. Jeff Greenberg, on the premise of delivering advanced primary care at scale, with financial skin in the game. Firefly fully embraced telehealth, asynchronous care models, and remote monitoring far before the COVID-19 pandemic, and even more importantly, they were one of the first virtual-first primary care groups to enter into value-based risk contracts (versus fee-for-service) for commercially-insured populations.
Firefly has also innovated on the way it partners with world-renowned specialty hospitals like Dana Farber Cancer Institute and Joslin Diabetes Center to deliver virtual-first specialty care at national scale, as well as brick and mortar facility partners to ensure that patients can be seen in person when needed or preferred. Their novel care model has already demonstrated substantial savings (e.g. 2x reduction in monthly cost per patient), elimination of unnecessary utilization (e.g. 52% reduction in emergency department visits), improvement in patient outcomes (e.g. 80% of hypertension patients in control of their blood pressure), and superior patient satisfaction (e.g. net promoter score (NPS) of 91).
Unlike most insurance products that focus on the administrative layers of the stack and then bolt on third-party care delivery services as an afterthought, Firefly started with a foundation in primary care, before evolving into a full-stack benefit to capture the full value of the care being delivered. Thus, they are poised to be a true healthcare quarterback to the 156M+ Americans covered by employer-sponsored health benefits, and the 13M+ consumers purchasing individual insurance on the exchanges, who are seeking a simpler, more convenient way to get high-quality healthcare, at half the price.
To that end, I couldn’t be more excited to be leading Firefly Health’s Series B, joining the board, and partnering with CEO Fay Rotenberg and her exceptional team to lead the charge on delivering transformative healthcare benefits, with a basis in transformative primary care.
* * *